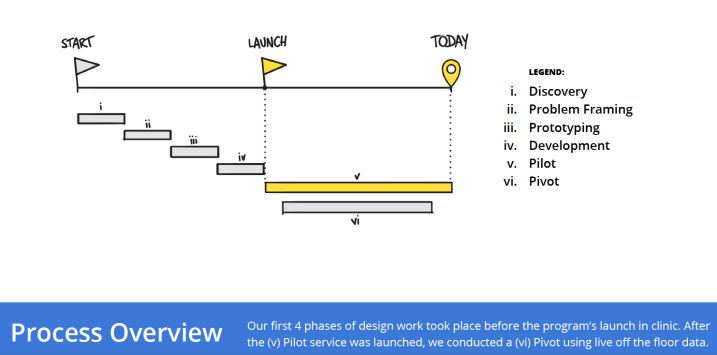
Process Overview
Our team carried out a 6 phase design process: (i) discovery (ii) problem framing (iii) prototyping (iv) development (v) pilot and (vi) pivot. This process immersed us into the lives of people grappling with this chronic deteriorating condition, it gave us exposure into a world-renowned cardiac clinic constantly abuzz with clinicians, patients, and families, and it saw us continuously iterate on an HF service until we were confident we had designed one that would not only stick, but that would transform the delivery of care.
(i) Discovery: We began by immersing ourselves into the world of chronic condition management and remote patient monitoring through an in-depth literature review and conversations with experts in this space. We then spent an entire week in the cardiac clinic observing what happens day-in and day-out, with a focus on understanding the culture of the clinic, the ways in which people work, the ways in which people experience care, and the blockers and facilitators of change.
To contextualize our learnings, we then interviewed 12 clinicians and administrators, and 24 patients, to dive more deeply into the nuances of their individual experiences.
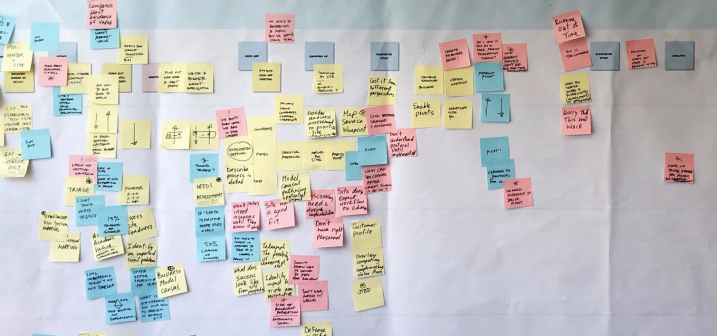
(ii) Problem Framing: The critical insight that emerged from our discovery was that there was a tension between the patients’ need to be cared for through the ups and downs of their illness, and the constant pressure that care teams were feeling in a clinic that was seeing increasing patient volumes and budgetary constraints.
This was the moment in which we realized that the service that supported the digital tool we hoped to design, was of more importance than the digital tool itself. As a digital system, in the absence of a service that is intentionally crafted with an in-depth understanding of the culture of the clinic, and of the needs of the patient, would never achieve adoption and ultimately improve the lives of patients.
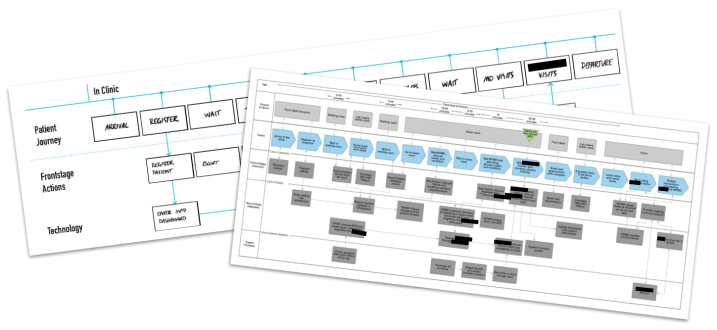
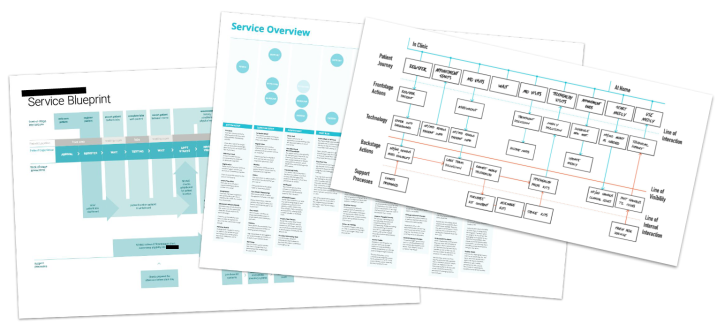
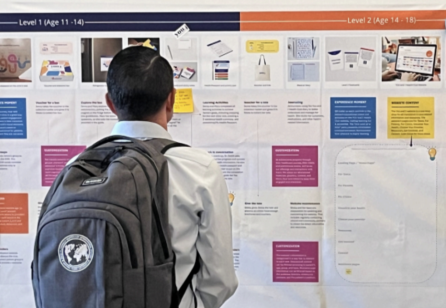
This insight, and others, were framed through a current-stage service blueprint, a suite of challenge statements, and design principles to guide the development of a digital tool to support patient self-care.
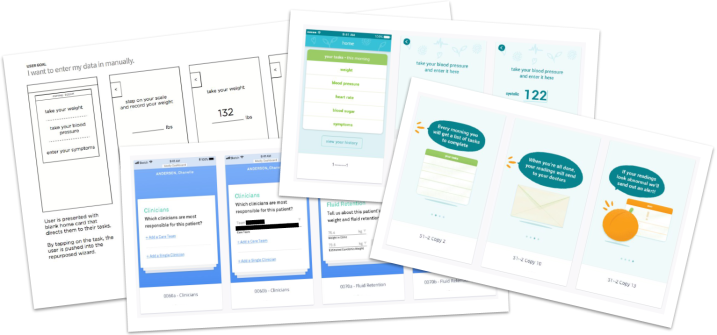
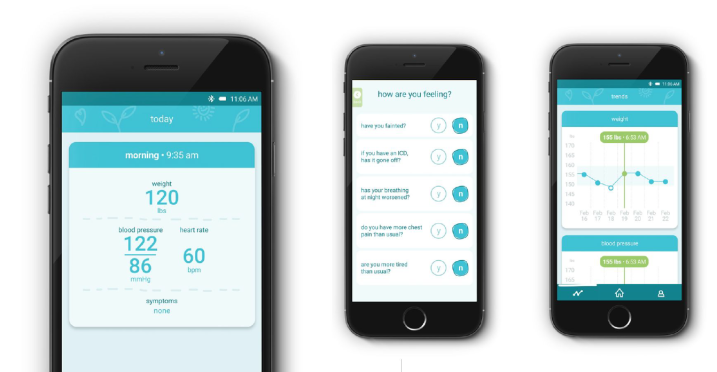
(iii) Prototyping: After our synthesis, we quickly moved to building, testing and improving the digital tool and accompanying service. By designing clickable prototypes and by staging the overarching HF service, we were able to quickly understand the ways in which clinicians diagnose and manage patient instability,
the ways in which patients experience their heart failure at home, and the drivers and blockers of adoption.
This enabled us to ensure that the service we designed allowed clinicians to identify at risk patients as quickly as possible, that it integrated into clinical workflow, and that it fit into the day-to-day activities of a patient’s life.








Share your thoughts
0 RepliesPlease login to comment